Evaluation of indirect indices in the insulin resistance assessment in patients with different body mass index
DOI:
https://doi.org/10.17532/jhsci.2024.2673Keywords:
Insulin resistance, homeostatic model assessment for insulin resistance, triglyceride to glucose index, triglyceride to glucose index-body mass indexAbstract
Introduction: Insulin resistance (IR) is a complex pathophysiological condition with multifactorial etiology characterized by a reduced responsiveness of target tissues to insulin (INS). Indirect indices based on mathematical models and derived from laboratory parameters have become increasingly popular in the past two decades. In this study, we evaluated their ability to predict IR in a population with different body mass index (BMI).
Methods: The matched case–control study was conducted in 2021 and 2022. Secondary data from 129 subjects were obtained from medical records, including demographic characteristics, anthropometric measurements, and biochemical laboratory test results. The studied group consisted of 91 subjects with a suspected diagnosis of IR who were further categorized according to BMI, while control group consisted from 38 age- and gender-matched subjects. Six widely used indirect indices were calculated: Homeostatic Model Assessment for IR (HOMA-IR), quantitative insulin sensitivity check index (QUICKI), McAuley index (MCAi), metabolic score for IR (METS-IR), triglyceride to glucose index (TyG), and TyG to BMI (TyG-BMI).
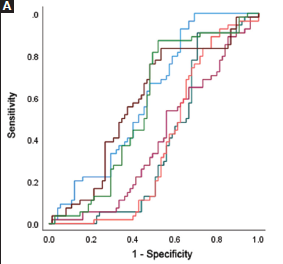
Results: Significant differences between the subgroups were found in the mean values for HOMA-IR, TyG, TyG-BMI, and METS- IR, while the control group had the highest mean values for the indirect indices QUICKI and MCAi (p < 0.001). HOMA-IR, TyG, and TyG-BMI showed statistical significance in predicting IR regardless of BMI (p < 0.05). In the obese group, TyG-BMI had good predictive power for discriminating IR (area under the curve [AUC] = 0.820), with a sensitivity and specificity of 84.1% and 87.7%, respectively. HOMA-IR showed moderate predictive power to discriminate IR in the obese group (AUC = 0.720), with a sensitivity and specificity of 70.4% and 89.1%, respectively.
Conclusion: As IR is a multifactorial disease, indirect indices combining laboratory and anthropometric data can significantly help in predicting and mitigating complications.
Downloads
Downloads
Published
License
Copyright (c) 2024 Lejla Čano Dedić, Arzija Pašalić, Emsel Papić, Emir Begagić, Sabina Šečić Selimović , Mario Gazibarić, Sabina Šegalo

This work is licensed under a Creative Commons Attribution 4.0 International License.